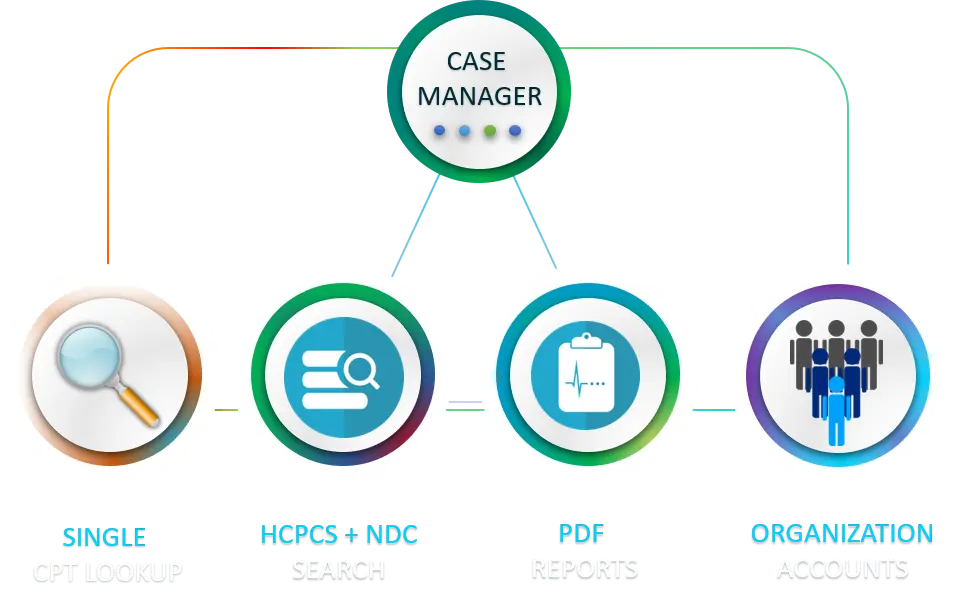
Coding and Billing
Inside the Medical Billing and Coding Labyrinth
Unbundling (Don’t pay twice!)
Description
The focus of this common issue is targeting claims where the procedure code includes imaging and imaging is billing separately. This is known as unbundlng.
The following is one example.
Affected Code(s)
CPT 79999 is Radiopharmaceutical therapy
CPT 70010 is a Myelography (imaging study)
Explanation:
In this case the imaging (70010) is included and paid within the therapy code (79999).
If unbundled (billed separately) the insurance company, Medicare or the patient is paying twice.
Correct Coding Initiative
In January 1996, CMS implemented the National Correct Coding Initiative (CCI). This initiative was developed to promote correct coding of health care services by providers and to prevent Medicare payment for improperly
coded services.
The CCI developed into a sophisticated system of coding checks that eliminate duplicate and unallowed payments. Commercial carriers and state Medicaid agencies also employ this system.
The most effective method of identifying these duplicate claims is to examine the EOB (explanation of benefits). That is the document that looks like the medical bill.
Look for a service that was billed, but no payment was allowed or paid. The amount billed (but not paid) is not a legitimate medical claim.

Contact Us Today To Book A Free Demo!
OFFICE HOURS
9 - 4:30pm
PST, M-F

HOME | CODING & BILLING | ABOUT | CONTACT | PRIVACY POLICY
valuetheclaim.com © 2025-2026 Washington Practice Management LLC.
